Dementia is a term commonly used to describe symptoms negatively affecting memory and thinking. There are many possible causes of dementia, including some reversible ones, depending on what is causing the brain injury responsible for the symptoms.
People living with HIV often suffer from cognitive problems, experiencing issues with memory, concentration and sometimes behavioral changes. In minor cases, people might cope adequately with these symptoms in their daily life. In a few cases, HIV can cause severe dementia, particularly if not treated, impairing one’s ability to live independently.
Detection
People living with HIV are susceptible to all forms of brain injury, just like people without HIV. That said, in order to make an accurate diagnosis of HIV-associated dementia, other causes of memory and concentration problems must be ruled out.
Reversible causes include substance abuse (e.g. sedative abuse), other central nervous system infections (e.g. encephalitis), vitamin deficiencies (e.g. vitamin B12 deficiency), psychiatric disorders (e.g. severe depression mimicking dementia) and hormonal imbalances (e.g. hypothyroidism). In these cases, once the cause is addressed, the cognitive problems might resolve.
Some forms of dementia are progressive and irreversible, such as Alzheimer’s or vascular dementia. Nonetheless, even in those cases, there are interventions that may slow down the progression, such as treating coexistent high blood pressure or diabetes.
Prevention
Untreated HIV infection can lead to brain damage, which in turn can cause dementia. The use of HIV medications, also known as antiretroviral medications, is essential in preventing and minimizing the damage HIV can cause to the brain. When someone is experiencing memory problems that could be caused by HIV infection, it is the physician’s job to assure the patient is indeed compliant with his or her antiretroviral regimen. It is also important to assure there is no viral resistance to the drugs being used, as this could indicate the need to switch to a different medication. HIV dementia may start with the person feeling depressed, lacking motivation or losing interest in activities with minimal impact on memory.
Preventing brain damage from HIV is a very good reason to justify early treatment of HIV infection, which was not always the standard of care, but is currently supported by Centers for Disease Control and Prevention (CDC) guidelines. It is crucial to remain adherent to the treatment, with regular medical follow-ups, to assure the current medications are working.
Sometimes, despite reassuring blood work and apparent successful treatment with an antiretroviral regimen, HIV is still detected in the cerebral spinal fluid (the fluid surrounding the brain) and therefore can theoretically cause brain damage.
Dr. Marcos C. Schechter, M.D., an Infectious Disease Fellow at Emory University, shed additional light on HIV-associated dementia's causes and treatments.
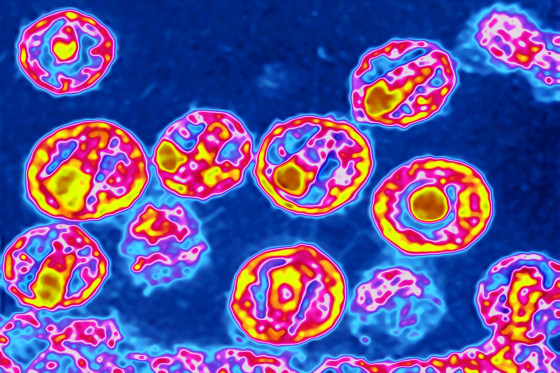
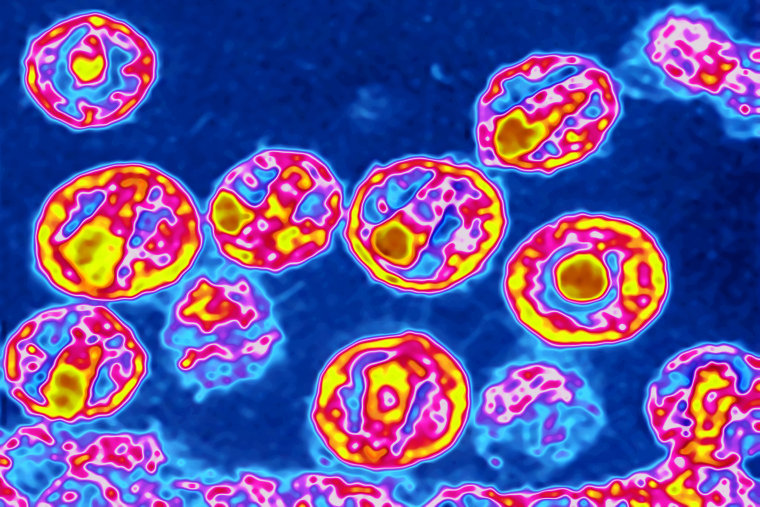
“HIV does infect brain macrophages (a type of cell involved in immune function), leading to an inflammation that is responsible for damaging the neurons. However, the presence of detectable viruses in the spinal fluid does not necessarily predict presence or development of cognitive problems,” Dr. Schechter said.
In other words, the fact that a patient might still have HIV detectable in the spinal fluid does not mean this person will develop HIV-associated dementia.
While doing a spinal tap to check the cerebral fluid for the presence of HIV viruses is not a test routinely done nor widely available, Dr. Schechter said it can be useful in some specific cases. A few people experience a scenario known as “central nervous system escape syndrome,” in which they experience rapid memory deterioration despite apparently well-controlled HIV. In those cases, a spinal tap could be warranted, and it would typically show persistent detectable viruses in the spinal fluid. A suspicion of encephalitis (an infection of the brain) can also prompt the need for a spinal tap, particularly if the person has untreated HIV, which leaves the brain more susceptible to infections and can contribute to memory problems.
Treatment
Currently, there are many antiretroviral medications available to treat HIV infection. This allows doctors to tailor the treatment according to the patient’s needs. These medications have different properties, and some do not reach the spinal fluid as well as others. Theoretically, if a person has high numbers of HIV viruses in the spinal fluid, despite compliance with antiretroviral medications and no detectable HIV viruses in the blood, it might be advisable to change the antiretroviral to one that can more easily get into the cerebral spinal fluid. However, according to Dr. Schechter, more research is needed regarding this issue.
“Most experts would not choose antiretroviral solemnly based on how well they reach the brain, even for patients with mild memory problems, given the still paucity of research available,” Dr. Schechter emphasized. This can be one of the factors taken into account when deciding which antiretroviral to prescribe. On the other hand, in the rare occurrence of the “central nervous system escape syndrome,” choosing an antiretroviral that reaches the brain more easily may be advisable.
Neuropsychological testing can help establish the severity of the memory problems and functional impairments, and treatment with cognitive rehabilitation can help improve one’s quality of life. For those who develop significant behavioral problems and personality changes as a result of HIV-associated dementia, psychiatric treatment can be helpful.
Conclusion
It is important that people living with HIV and their loved ones are aware of the symptoms of HIV-associated dementia, so the appropriate diagnostic investigation and treatment can be initiated as soon as possible. Investigation might discover other non-HIV-related factors causing the memory problems. In other cases, careful investigation might conclude that a change in the antiretroviral medication regimen is warranted in order to stop brain damage. In any case, it is important to take complaints of memory problems seriously in people living with HIV, as many causes are reversible and others — even if not completely reversible — can be slowed down after appropriate diagnosis and treatment.
Daniel Linhares, M.D., is an assistant professor of psychiatry at Columbia University Medical Center and a fellow of the American Psychiatric Association.